|
Introduction
Due to the prolonged survival of human beings, systemic
atherosclerosis may be the major health problem in this
century, and its association with physical inactivity,
excess weight, smoking, and alcohol is collected under
the heading of metabolic syndrome (1, 2). The syndrome
is characterized by a low-grade chronic inflammatory
process on vascular endothelium all over the body (3).
The inflammatory process is particularly accelerated
by some factors including sedentary lifestyle, excess
weight, smoking, alcohol, chronic inflammation and infections,
and cancers (4, 5). The syndrome can be slowed down
with appropriate nonpharmaceutical approaches including
lifestyle changes, diet, exercise, cessation of smoking,
and withdrawal of alcohol (6). The syndrome contains
reversible indicators including overweight, white coat
hypertension, impaired fasting glucose, impaired glucose
tolerance, hyperlipoproteinemias, alcohol, and smoking
for the development of irreversible consequences including
obesity, hypertension (HT), type 2 diabetes mellitus,
chronic obstructive pulmonary disease, cirrhosis, chronic
renal disease, peripheric artery disease, coronary artery
disease (CAD), and stroke (7, 8). In another perspective,
the metabolic syndrome may be the most important disease
of human lifespan decreasing its quality and duration
at the moment. The syndrome has become increasingly
common all over the world, for instance 50 million people
in the United States are affected (9). The syndrome
induced accelerated atherosclerotic process all over
the body may be the leading cause of early aging, end-organ
failures, and premature death for both genders. For
example, CAD is the leading cause of death in developed
countries. Although the absolute negative effects of
excess weight on physical health (10), there are various
reports about relationships between body mass index
(BMI) and depression or psychiatric disorders including
anxiety and somatoform disorders in the literature (11-13).
We tried to understand whether or not there is a relationship
between excess weight and mental health.
Materials and Methods
Due to the prolonged survival
of human beings, systemic atherosclerosis may be the
major health problem in this century, and its association
with physical inactivity, excess weight, smoking, and
alcohol is collected under the heading of metabolic
syndrome (1, 2). The syndrome is characterized by a
low-grade chronic inflammatory process on vascular endothelium
all over the body (3). The inflammatory process is particularly
accelerated by some factors including sedentary lifestyle,
excess weight, smoking, alcohol, chronic inflammation
and infections, and cancers (4, 5). The syndrome can
be slowed down with appropriate nonpharmaceutical approaches
including lifestyle changes, diet, exercise, cessation
of smoking, and withdrawal of alcohol (6). The syndrome
contains reversible indicators including overweight,
white coat hypertension, impaired fasting glucose, impaired
glucose tolerance, hyperlipoproteinemias, alcohol, and
smoking for the development of irreversible consequences
including obesity, hypertension (HT), type 2 diabetes
mellitus, chronic obstructive pulmonary disease, cirrhosis,
chronic renal disease, peripheric artery disease, coronary
artery disease (CAD), and stroke (7, 8). In another
perspective, the metabolic syndrome may be the most
important disease of human lifespan decreasing its quality
and duration at the moment. The syndrome has become
increasingly common all over the world, for instance
50 million people in the United States are affected
(9). The syndrome induced accelerated atherosclerotic
process all over the body may be the leading cause of
early aging, end-organ failures, and premature death
for both genders. For example, CAD is the leading cause
of death in developed countries. Although the absolute
negative effects of excess weight on physical health
(10), there are various reports about relationships
between body mass index (BMI) and depression or psychiatric
disorders including anxiety and somatoform disorders
in the literature (11-13). We tried to understand whether
or not there is a relationship between excess weight
and mental health.
Results
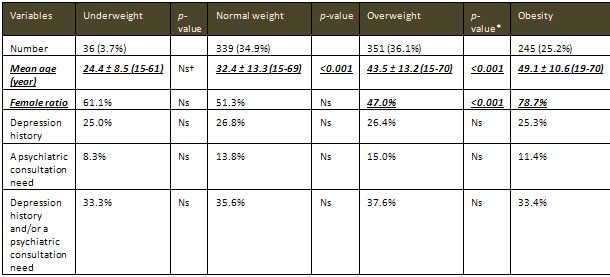
The study included 971
cases (554 females and 417 males), totally. There were
only thirty-six cases (3.7%) in the underweight group.
Prevalence of the cases with normal weight, overweight,
and obesity were detected as 34.9% (339 cases), 36.1%
(351 cases), and 25.2% (245 cases), respectively. Mean
ages of the groups showed gradual and highly significant
increases from the underweight towards the obesity groups
(24.4, 32.4, 43.5, and 49.1 years, respectively, p<0.001
nearly for all). The prominent but nonsignificant difference
between the underweight and normal weight groups according
to the mean age may just be due to the smaller sample
size of the underweight group. So aging alone may be
the main determinator factor of excess weight. Additionally,
female ratios were detected as 61.1%, 51.3%, 47.0%,
and 78.7% in the underweight, normal weight, overweight,
and obesity groups, respectively. So there was a significant
female predominance of the obesity group (p<0.001).
On the other hand, when we compared the four groups
according to history of medications for depression or
current need for a psychiatric consultation for any
cause, or both, there were not statistically significant
differences between them (p>0.05 for all) (Table
1).
Table 1: Characteristics of the study cases
Discussion
Probably obesity is found among one of the irreversible
endpoints of the metabolic syndrome, since after development
of obesity, nonpharmaceutical approaches provide limited
benefit either to heal obesity or to prevent its complications.
Overweight and obesity probably lead to a chronic low-grade
inflammation on vascular endothelium that is associated
with many coagulation and fibrinolytic abnormalities
suggesting that excess weight may cause a prothrombotic
and proinflammatory state (15). The chronic inflammatory
process is characterized by lipid-induced injury, invasion
of macrophages, proliferation of smooth muscle cells,
endothelial dysfunction, and increased atherogenicity
(16, 17). Elevation of C-reactive protein (CRP) levels
in serum carries predictive power for the development
of atherosclerotic end-points (18, 19), and overweight
and obesity are considered as strong factors for controlling
of CRP concentration in serum, because adipose tissue
produces biologically active leptin, tumor necrosis
factor-alpha, plasminogen activator inhibitor-1, and
adiponectin. So adipose tissue is involved in the regulation
of cytokines, and individuals with overweight and obesity
have elevated CRP levels in serum (20, 21). On the other
hand, individuals with excess weight will have an increased
circulating blood volume as well as an increased cardiac
output, thought to be the result of increased oxygen
demand of the extra tissue. The prolonged increase in
circulating blood volume may lead to myocardial hypertrophy
and decreased compliance, in addition to the common
comorbidity of atherosclerosis and HT. In addition to
the atherosclerosis and HT, fasting plasma glucose and
serum total cholesterol levels were all elevated with
the increased BMI values (22). Similarly, prevalence
of CAD and ischemic stroke increased with an elevated
BMI value in another study (23). On the other hand,
the chronic low-grade inflammatory process may also
cause genetic changes on the epithelial cells, and the
systemic atherosclerotic process may decrease clearance
of malignant cells by the immune system, effectively
(24). Eventually, the risk
of death from all causes including cardiovascular diseases
and cancers increased throughout the range of moderate
and severe weight excess for both genders in all age
groups (25).
Although the higher BMI is associated
with higher prevalence of atherosclerotic end-points,
there are various reports about its association with
psychiatric disorders . Some reports suggest the presence
of associations between atherosclerotic consequences
and psychiatric disorders, and these associations may
increase the likelihood of health service utilization
and length of stay in treatment programs (26). Mental
health tended to be related with the BMI (27), and there
was a higher prevalence of mental disorders among general
practice patients showing a BMI of 30 kg/m2 or higher
(28). Similarly, obesity was related with the increased
rates of mental disorders in women between the ages
of 18 and 25 years (29). Additionally, people with a
BMI of 30 kg/m2 or higher showed higher odds for depression
in a study performed among 50 to 94 year olds from Alameda
County (30). In another study, obesity was associated
with a 37% increase in the probability of being diagnosed
with major depression in women, while with a decrease
of similar magnitude in men (13). The positive association
between the relative body weight and probability of
major depression among adult women was additionally
shown with some previous studies by using subclinical
indexes of psychological well-being (31, 32). Similarly,
individuals with a lifetime history of major depression
were more likely to have obesity (19% versus 15%, respectively,
p<0.001), and lifetime major depression was associated
with higher odds of obesity in female respondents, whereas
not in male respondents as a result of sex-specific
multivariate analysis (33). In another study, obesity
was associated with significant increases in lifetime
diagnosis of major depression, bipolar disorder, and
panic disorder or agoraphobia (34). Additionally, a
10-unit increase of BMI increased the risk of past-year
suicide thought and attempts by 22% in females, however,
reduced the risk by 26% and 55%, respectively, in males
(13). An interesting finding among men may be the association
between being underweight and having an increased probability
of clinical depression and suicidal tendencies. The
relationship between lower BMI and depression was previously
demonstrated in a community sample of young males (35).
When the authors analyzed weight status as a categorical
variable, the underweight men were 81% more likely to
have thoughts about suicide, 77% were more likely to
have attempted suicide, and 25% more likely to be clinically
depressed than average-weight men (13). According to
the above study performed on 2,064 women aged between
18 and 25 years in Germany, obese women suffered from
an anxiety disorder significantly more often (29). Eventually,
according to a current review, the most rigorous clinical
studies suggest those children and adolescents with
major depressive disorder may be at increased risk for
developing overweight , patients with bipolar disorder
may have elevated rates of overweight, obesity, and
abdominal obesity, and obese individuals desiring weight-loss
therapy may have elevated rates of depressive and bipolar
disorders (36). According to the same review, the most
rigorous community studies suggest those depression
patients with atypical symptoms in females is significantly
more associated with overweight, obesity is associated
with major depressive disorder in females, and abdominal
obesity may be associated with depressive symptoms in
both genders, but most overweight and obese individuals
in the community do not have mood disorders (36). On
the other hand, similar to our results, another survey
study did not find a relationship between higher BMI
and general psychopathology by using the Diagnostic
and Statistical Manual for Mental Disorders IV criteria
based on the Composite International Diagnostic Interview,
and this study was conducted with a general population
sample of 3,021 German subjects ranging from 14 to 24
years of age and controlled for eating disorders (12).
There was not any significant association between the
higher BMI and mood, anxiety, substance use, and somatoform
disorders (12). Additionally, neither obesity nor underweight
was significantly associated with any kind of general
psychopathology (12). In another study, although authors
found a statistically significant relationship between
higher BMI and physical health, they could not between
the higher BMI and psychosocial outcomes such as poorer
emotional, school, or social functioning (37). Additionally,
obesity was associated with significantly lower lifetime
risk of substance use disorder both in males and females
(34). So although the sedentary lifestyle, excess weight,
smoking, alcohol, chronic infection and inflammation,
and cancers induced chronic low-grade inflammatory process
on vascular endothelium all over the body may shorten
the human lifespan significantly, there is not any significant
association between the inflammatory process and mental
health in general.
In the absence of any chronic
low-grade inflammatory background of mental health on
vascular endothelium, our results about the effects
of under- and excess weight on mental health may also
be explained by the self-admiring properties of the
human being. Human beings believe that their features
are the best for themselves. He or she is created as
the best, and he or she is actually the wonderful person
in the world. Their height, weight, and intelligence
are actually the optimum for themselves. Thus he or
she is afraid of changing image or body compositon,
actually. This property may be necessary for human beings
to be able to live and fight against various stresses
during their lifespan. In the absence of this property,
human beings may not be able to fight against various
stresses and continue to survive during their lifespan,
and they may desire to terminate their lives frequently.
So although the self-admiring property of human beings
seem bad, it may be absolutely necessary to be able
to continue his or her life in this stressful world.
As a conclusion, metabolic syndrome
is a chronic low-grade inflammatory process on vascular
endothelium all over the body, terminating with an accelerated
atherosclerosis, early aging, end-organ failures, and
premature death. Although excess weight is the main
determining factor of the syndrome, neither under- nor
excess weight has any adverse effect on mental health.
So mental health may not have a chronic low-grade inflammatory
background on vascular endothelium in general.
References
1. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome.
Lancet 2005; 365: 1415-1428.
2. Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr,
Lenfant C. Definition of metabolic syndrome: Report
of the National Heart, Lung, and Blood Institute/American
Heart Association conference on scientific issues related
to definition. Circulation 2004; 109: 433-438.
3. Tonkin AM. The metabolic syndrome(s)? Curr Atheroscler
Rep 2004; 6: 165-166.
4. Helvaci MR, Kaya H, Seyhanli M, Cosar E. White coat
hypertension is associated with a greater all-cause
mortality. J Health Sci 2007; 53: 156-160.
5. Helvaci MR, Kaya H, Duru M, Yalcin A. What is the
relationship between white coat hypertension and dyslipidemia?
Int Heart J 2008; 49: 87-93.
6. Helvaci MR, Aydin LY, Aydin Y. Chronic obstructive
pulmonary disease may be one of the terminal end points
of metabolic syndrome. Pak J Med Sci 2012; 28: 376-379.
7. Helvaci MR, Kaya H, Gundogdu M. Gender differences
in coronary heart disease in Turkey. Pak J Med Sci 2012;
28: 40-44.
8. Helvaci MR, Seyhanli M. What a high prevalence of
white coat hypertension in society! Intern Med 2006;
45: 671-674.
9. Clark LT, El-Atat F. Metabolic Syndrome in African
Americans: implications for preventing coronary heart
disease. Clin Cardiol 2007; 30: 161-164.
10. Allison DB, Pi-Sunyer FX. Obesity treatment: examining
the premises. Endocr Pract 1995; 1: 353-364.
11. de Graaf R, Bijl RV, Smit F, Vollebergh WA, Spijker
J. Risk factors for 12-month comorbidity of mood, anxiety,
and substance use disorders: findings from the Netherlands
Mental Health Survey and Incidence Study. Am J Psychiatry
2002; 159: 620-629.
12. Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel
AW. Are obese adolescents and young adults at higher
risk for mental disorders? A community survey. Obes
Res 2002; 10: 1152-1160.
13. Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships
between obesity and DSM-IV major depressive disorder,
suicide ideation, and suicide attempts: results from
a general population study. Am J Public Health 2000;
90: 251-257.
14. Third Report of the National Cholesterol Education
Program (NCEP) Expert Panel on Detection, Evaluation,
and Treatment of High Blood Cholesterol in Adults (Adult
Treatment Panel III) final report. Circulation 2002;
106: 3143-3421.
15. De Pergola G, Pannacciulli N. Coagulation and fibrinolysis
abnormalities in obesity. J Endocrinol Invest 2002;
25: 899-904.
|